Case Reports
Rectus abdominis overuse injury in a tennis athlete treated with Traumeel injections
K. Natsis, Chr. Lyrtzis, E. Papathanasiou, N. Anastasopoulos published in Am J Case Rep, 2012; 13: 3-6.57
Traumatic musculoskeletal pathology is frequent in athletes. Muscle injuries account for more than 30% of sport injuries. One of the more common injuries is a muscle strain. A strain causes microscopic tears within the muscle, but occasionally, in severe injuries, the muscle can be ruptured. The most frequent cause of partial or complete rupture of muscle is the eccentric overload of the muscle or muscle overstretching. Severe muscle strains can lead to hematoma formation.
This case report covers a case of an overuse injury of the rectus abdominis muscle following overstretching during a tennis service in an athlete treated with injection of Traumeel Injection Solution and modification of the serve technique.
A 21-year-old female tennis champion was injured on her abdominal wall during a service in competition play. Specifically, she felt pain on her contralateral of service abdomen after a service but did not stop playing. She continued to suffer from pain in her abdomen and tenderness with any attempt of movement. Her trainer observed a tender mass after the trauma and he tried to control the pain with ice packs in the field. She was not initially restricted from athletic competition. One week later, again during a service, she experienced severe pain in her abdomen.
Conservative treatment was performed by a team physician with rest, ice therapy and analgesics for 20 days. There was an improvement and she decided to participate in training. During the first day of training she felt the same pain during service. Conservative treatment was performed for 20 days with rest, ice application, anti-inflammatory medication, muscle relaxant drugs, ultrasound and iontophoresis, followed by active stretching of the muscle within the athlete’s pain limits and isometric exercises.
She was instructed to perform active, pain-free rectus abdominis stretching 15 times a day and to perform pain-free isometric rectus abdominis strengthening exercises. She started training and after 2 days she felt the same pain during the service. Three months after the initial injury and following a new injury, she underwent clinical examination in another clinic, where a hematoma in the left rectus abdominis muscle was found that was 7×2×3 cm.
The patient was not on any medication and had no known blood disorders. Due to the recurrence of symptoms and failure of conventional treatment, the physicians decided to modify the standardized treatment protocol and to use Traumeel Injection Solution.
The patient was treated under aseptic conditions, with injection of Traumeel. The hematoma was palpated and 2 ampules of Traumeel Injection Solution were injected. The hematoma was not aspirated before injection. The treatment was administered on the 2nd, 4th, 6th post-traumatic days and 1 injection on the 10th post-traumatic day. The goals of treatment included pain-free rectus abdominis flexion and extension and unrestricted return to full athletic activities as soon as possible.
After 3 weeks of treatment the athlete started training and a rehabilitation program including controlled warm-up and muscle stretching. MRI revealed a nearly complete recovery and she had pain-free function. The patient was instructed to modify the service technique in cooperation with her trainer and returned to her former sport activities and competitions. Two years later there is no recurrence of her injury and she participates under competition conditions in her sport. In this case Traumeel injections and modification of service technique were effective and no recurrence of rectus abdominis muscle strain was reported at 2-year follow-up. The combination of Traumeel injections and modification of service technique can be used for treatment of rectus abdominis overuse injuries according to the authors.
A case of lateral epicondylitis
Dr Alvaro Maúrtua Briseño-Meigss, Magdalena Health Center, Valladolid, Spain (unpublished report)
The patient described in this case report is a 33-year-old male elite athlete (tennis player and marathon runner) who had recurrent pain and limited movement in his right elbow due to overuse rather than to direct trauma.He had previously received conventional non-steroidal anti-inflammatory drugs and had developed gastro-esophageal reflux disease as a consequence. Physical examination revealed pain, swelling, increased local temperature and limited flexion-extension.
Over a period of up to 4 weeks, a questionnaire was administered to assess the following: elbow circumference, local skin temperature, muscle function, pain (based on a Visual Analog Scale of 1–10), opinion of the treatment (improvement, no change). The diagnosis was right lateral epicondylitis. Treatment consisted of Traumeel injection into the elbow (1 ampule every 8 hours).
Traumeel injections reduced elbow swelling, local skin temperature, and pain. Normal function and sports activities were resumed rapidly after the start of treatment. The patient reported improvement in retrosternal heartburn and epigastric pain (signs of gastro-esophageal reflux disease). Traumeel Injection Solution provided an effective alternative to non-steroidal anti-inflammatory drugs and was well tolerated. The patient considered that his condition was fully resolved.
A case of acute trochanteritis
Dr Joaquín Carreño Renduelles, Capua Private Clinic, Gijón, Spain (Unpublished report)
Two female patients aged 17 and 18 years, respectively, with pain in the left hip. Both patients participated in sports activities (handball and basketball) and reported that pain prevented training.On clinical examination, both women had tenderness in the greater trochanter, pain on external hip rotation, and pain on thigh flexion. Radiographic assessment of the hip to rule out necrosis of the femoral head (because of patient age, pain in the area of the coxofemoral joint, and overload of these joints in such athletes). Functional limitation was evaluated based on a Visual Analog Scale for pain and on the ability to perform usual sports training. At baseline, tenderness in the greater trochanter was rated a VAS score of 7, pain on external hip rotation was rated a VAS score of 8–10, and pain on thigh flexion was rated a VAS score of 7–10.
Acute trochanteritis in the left hip due to overload was diagnosed. The treatment consisted of Traumeel injection: 1 ampoule every 3 days in the first week, followed by 1 ampoule weekly for 2 weeks, administered as a fan-like subdermal injection in the area of the greater trochanter of the left femur.
After 1 week of treatment, the Visual Analog Scale pain score decreased by 2–3 points. Physical work of the lower body was resumed; patients could jog, but were to avoid multiple jumps and changes of pace.
After 3 weeks (injection therapy completed), the VAS pain score had further decreased to 2 on palpation and on thigh mobilization against resistance. Patients returned to training and reported minor discomfort (VAS pain score of 3) during training that did not inhibit usual activity.
After 2 months, patients continued activities with minimal discomfort (VAS pain score of 1) and without problems. Therapy encouraged treatment adherence; injections caused little discomfort and did not alter daily schedules, while the ointment was easy to administer.
A case of patella tendonitis
Izabela Fołta MD, NZOZ-Vitamed Chylonia Medical Clinic, Gdynia, Poland (Unpublished report)
A 37-year-old soldier who had complained for several days of severe pain, warmth and swelling of the left knee. The problem had arisen the day after a visit to the beach where he participated in sports and long walks on the sand. His general practitioner had prescribed an oral non-steroidal anti-inflammatory drug (diclofenac), but there had been little improvement.On examination, there was swelling primarily in the area below the left knee and local warming. He experienced intense pain when trying to straighten the leg and on palpation. There was no internal fluid accumulation. Radiological examination did not show any pathological changes to the knee joint. Patellar tendonitis, particularly around the attachment to the shin bone was diagnosed.
The treatment consisted of Traumeel injection around the patellar tendon and its attachment: 1 ampule on days 1, 4 and 6. To support the healing. Movement of the knee was restricted.
Subjective improvement occurred a few hours after the first injection of Traumeel. At the first check-up, pain on movement and swelling of the knee were considerably reduced. The soldier returned to military service. The physician observed that Traumeel Injection Solution had a fast clinical effect, with improvement noted a few hours after the first injection. Traumeel Injection Solution was effective in reducing pain and swelling of the knee, whereas an oral non-steroidal anti-inflammatory drug (NSAIDs, diclofenac) had provided little improvement.
Two cases of quadriceps aponeurosis
Dr Marcin Domżalski, Dr Z. Radliński’s Provincial Center of Orthopedics and Rehabilitation, Łódź, Poland (Unpublished report).
A 26-year-old male professional volleyball player who had complained for 6 months of pain during exertion on both sides of the patella anterior to the patella base. On palpation, he had pain at the base of the patella. He had a normal range of movement of the knee joint, which was stable and without exudation. The patella showed normal shifting and an undisturbed movement path. Meniscus tests were negative. Enthesopathy and overload inflammation of the quadriceps aponeurosis were observed. Damage was an element of “jumper’s knee”, an overload syndrome of the extensor apparatus of the knee joint that may also lead to damage of the patella ligaments.Further ultrasound examination showed thickening of the quadriceps aponeurosis at the attachment to the base of the patella (9 mm compared with the normal mean value on extension of 6.5 mm, and 8.5 mm for tendons with an inflammatory reaction) (Figure 1).
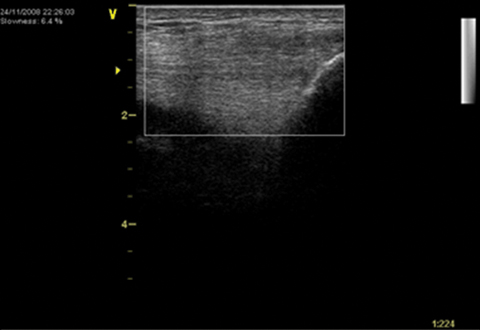
Figure 1: Ultrasound of the affected area
Local damage of aponeurosis fibers with the presence of hypoechogenic regions was also observed. Small deposits of calcification near the base of the patella indicated an intensified enthesopathic process B-flow coded ultrasound revealed proliferation of blood vessels penetrating into the aponeurosis, particularly approximately 10 mm anterior to the patella base.
The condition was treated with Traumeel injection in the aponeurosis region: 1 ampule every 3 days for 2 weeks. Training activity was prohibited during the two weeks of therapy.
At 3 weeks, there was a reduction in overall pain (Visual Analogue Scale score reduced from 7 to 2). Pain was not interfering with his training schedule anymore and stopped limiting participation in his athletic profession. Traumeel Injection Solution provided an effective and well-tolerated treatment of pain related to overload damage of the quadriceps aponeurosis.
The second case was a 35-year-old male international body-builder who had complained for many months of pain during exertion on both sides of the patella in an anterior direction from the patella base. On palpation, he had pain at the base of the patella. He had a normal range of movement of the knee joint, which was stable and without exudation. The patella showed normal shifting and an undisturbed movement path and meniscus tests were negative. Radiological examination of the knee joint was normal. Ultrasound examination showed thickening of the quadriceps aponeurosis at the attachment to the base of the patella (10 mm compared with the normal mean value on extension of 6.5 mm, and 8.5 mm for tendons with an inflammatory reaction) (Figure 2).
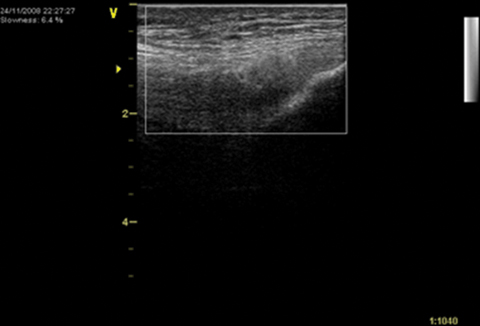
Figure 2: Ultrasound of the affected area
The diagnosis was Enthesopathy and overload inflammation of the quadriceps aponeurosis.
The treatment consisted of Traumeel injections into the aponeurosis region: 1 ampoule every 3 days for 2 weeks
At 3 weeks, there was a reduction in overall pain (Visual Analog Scale score reduced from 8 to 2) that allowed the patient to start training again.
A case of Achilles tendon pain
Dr Marcin Domżalski, Dr Z. Radliński’s Provincial Center of Orthopedics and Rehabilitation, Łódź, Poland (Unpublished report).
A 24-year-old female track-and-field athlete who had complained for several weeks of pain in the area around the Achilles tendon. The pain disappeared for two days after physical therapy but returned with training. On palpation, she had pain at the site of tendon attachment to the calcaneal tuber and on pressure to the tendon, particularly about 2 cm below the calcaneal tuber. A tendon pressure test was positive only during maximum plantar bending in the ankle, suggesting that the pain originated in the mid-tendon. She also complained of pain during standing and walking on tip-toe. Ultrasound examination showed thickening of the Achilles tendon, with a visible tissue reaction near the tendon sheath. Fibrous tissue proliferation had altered the tendon architecture, particularly about 2 cm below the calcaneal tuber.Examinations using doppler and a B-flow coded ultrasound technique revealed significant proliferation of blood vessels within the Achilles tendon, indicating an advanced degenerative process and chronic inflammatory reaction.
The final diagnosis was overload damage, with resulting degeneration of the Achilles tendon.
The treatment consisted of Traumeel injection at the most painful site beneath the Achilles tendon: 1 ampule every 2 days for three weeks. The athlete was suspended from training for the course of the treatment.
Follow-up at 4 weeks after the athlete had resumed training revealed: reduction in overall pain (Visual Analogue Scale score reduced from 7 to 3). Reduction in pain on palpation of the Achilles tendon and no pain on power and movement exercises on the toes. Because of the detected degenerative changes, continued monitoring was recommended.
Traumeel Injection Solution provided effective and well-tolerated treatment of pain associated with overload damage to the Achilles tendon. Pain was rapidly reduced, enabling training to be resumed after 3 weeks.
Complex strain injury involving an intercostal hematoma in a professional baseball player
M. L. O’Neal, DO, K. McCown, MD, and G. C. Poulis, MA, ATC/L published in Clin J Sport Med 2008;18:372–373.59
An elite, left-handed Major League Baseball player originally experienced mild, right-sided thoracic ‘‘soreness’’ after swinging a bat. There was mild tenderness at the anterolateral 10th intercostal space. The athlete experienced slight exacerbation of pain during deep inspiration with no discomfort with active or passive rotation.These clinical findings were consistent with an intercostal strain. The patient was not initially restricted from athletic participation. Two days later, again while batting, he immediately experienced severe and ‘‘sharp’’ pain in the right, lower thoracic region. During examination, a tender, palpable mass was noted at the anterolateral 10th intercostal space. In addition to more severe pain during inspiration, the discomfort was also exacerbated by rotation and side-bending, which limited his ability to participate in athletic activities for nearly 1 month. Initial chest radiographs were negative. There was negligible improvement with conservative measures (rest, anti-inflammatory medication, ultrasound, iontophoresis) during this convalescent period, which lasted 30 days.
Magnetic resonance imaging (MRI) of the chest was ordered because of the athlete’s delayed recovery despite measures that would typically be considered adequate for a simple strain. This study revealed signal-intensity changes within the right internal intercostal muscle between the tip of the 11th rib and the 10th costal cartilage, suggestive of a focal tear of the intercostal muscle with hematoma. There was also signal-intensity change (without organized hematoma) in the right internal oblique muscle just inferior to the intercostal injury, which represented concomitant muscle strain.
Four weeks following the initial injury, the patient opted for an alternative therapy and received an intralesional injection into the involved intercostal space with Traumeel injections solution. The hematoma was not aspirated.
Within 3 days following injection, he was capable of returning to unrestricted activity and has remained pain free without limitations or recurrent injury after 3 years.
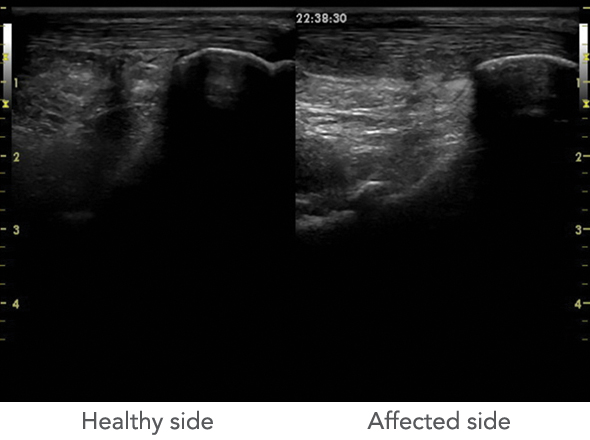
Figure: Ultrasound picture of the affected and the healthy side.
Treating a dancer with posterior ‘impingement’ pain
Lisa M. Schoene, DPM, ATC published in Podiatry Today, Volume 26 - Issue 1 - January 2013.60
A professional dancer presented with pain in the right plantar heel that she had for two weeks and right posterior heel pain deep in the Achilles tendon area that she had experienced for approximately four weeks. The plantar and posterior heel areas were both sore and achy in nature, and aggravated by increased activities and dancing in the morning and after prolonged sitting. The Achilles had been sore for a longer timeframe and at times the ankle felt “jammed” and “stiff with full relevé and plié positions.” The patient denied any ecchymosis, warmth or neurological type pain or symptoms. There was no swelling plantarly but slight fullness in the posterior heel area along the anterior border of the Achilles tendon.The patient was dancing every day, typically in ballet slippers or barefoot, which aggravates both areas of pain. There was some previous and current lateral leg muscular soreness along both muscle bellies. She noted she had some relief of these issues with massages and strengthening exercises. A physical therapist had treated the patient at the dance studio with ultrasound, massage and various taping methods.
The physical exam revealed pain with palpation at the medial plantar heel with no swelling, color or warmth. The patient’s initial treatment after thorough differential diagnosis was a corticosteroid injection into plantar heel. In order to address both pain locations, a combination of strapping with a dancer’s pad was applied, as well as the use of heel cups with heeled shoes, stretching, ice, physical therapy modalities and massage to the lateral and medial extrinsic foot musculature. In regard to dance modification, the patient was advised to limit jumping and had her wear jazz shoes or dance gym shoes with padding/heel cups and/or tape.
Due to the patient's work travel and performance schedule, the first follow-up was at 12 weeks. The patient had full plantar heel pain resolution due to exceptional adherence. The posterior heel/Achilles area was still painful to palpation with persistent minimal swelling in the retrocalcaneal bursa area. She felt much better in heeled shoes and any flat shoes or barefoot dancing were painful as the posterior heel pain was re-aggravated, even with various persistent treatments.
In addition to repeating the aforementioned treatments, the patient also received a Traumeel injection into the posterior heel/bursa/Achilles area. The use of diagnostic ultrasound revealed the following findings: A mild increase in caliber to the Achilles tendon, watershed area and distally posterior to the calcaneus, a small focal deficit (4 mm x 4 mm x 2 mm) to the anterior fibers of the Achilles at the posterior superior corner of the calcaneus, a prominent posterior superior border of the calcaneus with some impingement of the anterior fibers of the Achilles with dynamic evaluation. There was also hypertrophy of the retrocalcaneal bursa with increased fluid observed, as well as a slight extension of the peroneus brevis muscle belly distal to the inferior aspect of the lateral malleolus with significantly hypertrophy.
The treatment continued with a series of Traumeel injections into damaged tissues: Bimonthly injections in combination with deep tissue work, ultrasound, heat, heeled shoes and modified dancing with some form of heel padding. In addition to performing continued strengthening exercises, the patient also ensured proper warm up and cool down periods. Although this dancer has a “posterior” condition, she felt best with some slight heel height in her street shoes but excessive relevé and plié positions were uncomfortable.
The physician focused on repairing the Achilles tendon and reducing inflammation of the bursa via conservative needling. By applying a series of injections into damaged tissues the inflammatory cascade can be stimulated to induce reorganization of the disorganized collagen type III into proper type I collagen, creating the best linear mechanical strength for the tendon. The bimonthly injection of Traumeel Injection Solution created stability while still allowing mobility of the tendon, which is paramount to proper regeneration. These injections encourage the continual recruitment of fibroblasts to allow the tissues to go through more controlled inflammatory, proliferative and remodeling stages. Although these patients should ideally emphasize relative rest for the duration of the treatment protocol, this would be difficult for a professional dancer. This regimen affords the best outcomes with little to no downtime for the dancer's schedule with only minor compromises and alterations.
A case of Morton’s neuroma
Angela L. Drury D.P.M., F.A.C.F.A.S., Podiatric Medicine and Surgery, Albuquerque, New Mexico, USA published in Alternative Therapies, 2011, VOL. 17, NO. 2.61
A 70-year-old woman presented complaining of severe and constant pain in the ball of her foot, particularly when walking (Visual Analog Scale score 8 out of 10). She had been seen previously by podiatrists and received a cortisone injection and a series of alcohol sclerosing injections, none of which were effective. Surgery was scheduled. On examination, a swelling could be felt between the metatarsal heads. There was obvious splaying of the second and third phalanges, which worsened with weight bearing. On palpation, there was pain, swelling and tenderness.A positive “Mulder Click” (popping sound and sensation) was reproduced with lateral compression. Normal range of motion of the metatarsal-phalange joints was observed that did not cause pain. X-rays were negative for fracture and arthritis. Ultrasound was performed using an 18 MHz linear probe in B-mode with gray scale imaging. Both real-time and static images were taken. The final diagnosis was Morton’s neuroma.
Ultrasound guided Traumeel injections were administered: 1 ampule of Traumeel Injection Solution mixed with 1.5 cc of 0.25% marcaine (total fluid volume approximately 5 cc) given 10 times over 2 weeks. In addition, the patient was fitted for biomechanical orthotics (shoe inserts) and advised to limit activities.
The patient is free of pain and was able to continue with her normal activities. Use of Traumeel Injection Solution, ultrasound and shoe inserts avoided the need for surgery for Morton’s neuroma. Traumeel injections can be used as required, unlike corticosteroid injections which should not be given on more than 3 to 4 occasions per year.